Even before the Covid-19 pandemic, people were experiencing a loneliness epidemic. A 2018 Kaiser Family Foundation study revealed that one in five Americans said they always or often felt lonely or socially isolated. (1) Just as concerning, loneliness is associated with mental health issues like depression and anxiety; lower overall well-being around quality of life, satisfaction, sleep, and physical health complications. (2,3) When compared to other leading health indicators in the United States, loneliness impacts a greater number of adults than those classified as obese, severely obese, inactive, and smokers. (4) It doesn’t help that we are living in an age where we are surrounded by online connectivity, yet feel more isolated than ever. (5,6) Recent studies from the pandemic serve to reaffirm this. (7) The lack of in-person connection and community amongst neighbors, friends, and family is a symptom of our modernizing society, (8) yet our health depends on these human interactions just as much as when we were a tribal species millennia ago.
The health impacts of loneliness are especially prevalent in our aging population. The loss of purpose as we age, whether through an empty nest, retirement, or the passing of a spouse is often the watershed moment that highlights the need for a well-established community, and the consequences of its absence can be devastating. Multiple studies have shown the detrimental effects of loneliness and isolation on aging. It increases mortality, (9) decreases quality of life, (10) and has been shown to drive up healthcare costs and utilization. (11) So what can we do to address this at scale and help people live happier and longer lives?
Addressing the loneliness epidemic and improving health outcomes through a peer based community health approach.
Recognizing the growing need to improve loneliness and social isolation among vulnerable populations, in 2016 Wider Circle piloted a live, peer-based intervention called Connect for Life® (CFL) in select communities across California. Today, the CFL program has scaled to serve hundreds of vulnerable and underserved communities across 12 states on behalf of payers and providers that tackles loneliness, mental health, and other important health issues.
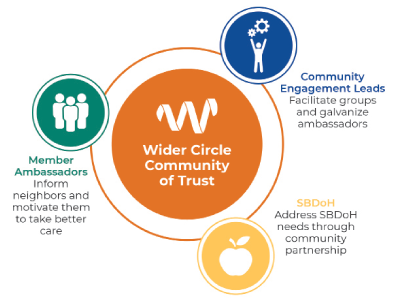
In the CFL program, Wider Circle community engagement specialists form and manage groups of members within a given neighborhood and recruit volunteer ambassadors to motivate their fellow members to take better care of their health and wellbeing. The goal is to create trusted peer-to-peer social connections, demonstrating the importance of preventative care and mental health, whilst also addressing social determinants of health (SDoH), barriers to obtaining care, and improving care navigation.
Critical to the model is the formation of long term relationships with multiple peers of similar backgrounds versus isolated visits or calls to plan members from strangers. The peer-to-peer engagement forum maximizes influence by allowing individuals to connect with society in comfortable ways, combining connection with credible information sources, and enabling members to become more astute consumers of health services in their own local context. The group cohesion and trust of those care communities increases and sustains the motivation of participants to take better ownership of their health.

Small groups of 12 enrollees participate in consecutive in-person and virtual, hour-long meetings led by a Wider Circle community engagement liaison, skilled in motivational interviewing techniques, who is sourced, trained, and managed by Wider Circle. Throughout the member journey, Wider Circle leverages the psychology of influence through using data to group similar individuals together and hiring local facilitators so they have culturally competent, consistent group dynamics that can pressure levers that will drive better health and address isolation.
Members become part of a larger community after completing their weekly meetings in the smaller group setting. As a part of that larger community, they are invited to participate in further meetings, group physical activities, or peer-to-peer local information exchanges about disease specific wellness resources for mental health and otherwise. Local chapter members are encouraged to rotate as activity leaders and integrate new chapter members into their community.
Six-month study demonstrates significant decreases in loneliness and increases the number of healthy days of participants
In order to quantify Wider Circle’s impact on loneliness they collaborated on a study with a health plan to survey Medicare members who participated in Connect for Life (CFL), defined as attending two or more events, versus those who hadn’t. They used two validated patient reported outcome (PRO) questionnaires, Health Related Quality of Life (HRQoL-2, also known as Healthy Days) and the UCLA 3-item loneliness scale (12) to ascertain members’ perception of their health and loneliness at baseline and 12 months later. 46,252 members were eligible for Wider Circle and randomized into treatment or control eligible groups. 711 members in the treatment group answered the baseline and follow up surveys and 254 members answered the control baseline and follow-up surveys. All participants were over age 65, resided in in Fulton, Dekalb, Clayton, or Gwinnett counties in GA and had one or more of the following chronic conditions: CAD / IHD, depression, CHF, COPD, diabetes, hypertension, hyperlipidemia, asthma, atrial fibrillation, and osteoporosis.

Results were analyzed using a logistic regression model. This adjusted for the break in initial randomization when moving treatment-eligible members to the control-eligible group and for differences in demographics and other variables among the two groups.
Wider Circle participants were 2.2 times more likely to have at least a 15% reduction in unhealthy days when compared to the control group (p<0.0001). Variables adjusted for in the logistic regression model included treatment, age, sex, race, disabled flag, language spoken, dual flag, and Charlson Comorbidity Index.
Again, using a logistic regression model, those who participated in Wider Circle were 3.8 times more likely to go from being lonely to not lonely during the study period compared to those in the control group (p<0.0001). To be classified as not lonely participants had to answer “hardly ever” to all three questions on the UCLA 3-item scale. If participants answered sometimes or often to any of the questions they were classified as still being lonely. Variables adjusted for in the logistic regression model included treatment, race, sex, dual flag, disabled flag, and Charlson Comorbidity Index score.
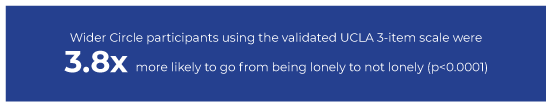
The results show that Wider Circle was able to provide significant improvement to members’ perception of loneliness.
Although it is not possible to attribute causality, it is plausible that through the increased odds of having decreased unhealthy days through Wider Circle program enrollment, there are cost savings and further ROI from the program. Wider Circle is actively scaling its CFL intervention for Medicare and Medicaid populations, continuing to address health issues, care gaps, and social determinants of health for risk bearing providers and payers. They operate across 12 states in the U.S. in five different languages. If you are interested in partnering with them, please get in touch.
To learn more, contact:
Claude Pinnock, MD, MPH
Chief Medical Officer, Wider Circle
cpinnock@widercircle.com
www.widercircle.com
1 DiJulio, Bianca. Hamel, Liz. Muñana, Cailey. Brodie, Mollyann. (2018). Loneliness and Social Isolation in the United States, the United Kingdom, and Japan: An International Survey. Retrieved July 6, 2022, from https://www.kff.org
2 Park, Caroline, MSc, et al. (2020) The Effect of Loneliness on Distinct Health Outcomes: A Comprehensive Review and Meta-Analysis. Retrieved July 21, 2022, from www.sciencedirect.com
3 Leigh-Hunt, N et al. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Retrieved July 9, 2022, from www.sciencedirect.com
4 Holt-Lunstad, Julianne , PhD. Robles Theodore, PhD. Sbarra, David A., PhD. (2017). Advancing Social Connection as a Public Health Priority in the United States. Retrieved July 9, 2022, from www.ncbi.nlm.nih.gov
5 Primack, Brain A., MD, PhD. (2017). Social Media Use and Perceived Social Isolation Among Young Adults in the U.S. Retrieved July 9, 2022, from www.ajpmonline.org
6 Nowland, Rebecca. Necka, Elizabeth A. Cacioppo, John T. (2017). Loneliness and Social Internet Use: Pathways to Reconnection in a Digital World? Retrieved July 11, 2022, from www.journals.sagepub.com
7 Pai, Nagesh. Vella, Shae-Leigh. (2021). COVID-19 and loneliness: A rapid systematic review. Retrieved July 11, 2022, from https://pubmed.ncbi.nlm.nih.gov
8 Boyd, Robert. Richerson, Peter J. (2009). Culture and the evolution of human cooperation. Retrieved July 11, 2022, from www.ncbi.nlm.nih.gov
9 Holt-Lunstad, Julianne. (2015). Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Retrieved July 11, 2022, from https://journals.sagepub.com
10 Musich, Shirley, et al. (2015). The Impact of Loneliness on Quality of Life and Patient Satisfaction Among Older, Sicker Adults. Retrieved July 11, 2022, from https://journals.sagepub.com
11 Gerst-Emerson, Kerstin PhD. Jayawardhana, Jayani, PhD. (2015). Loneliness as a Public Health Issue: The Impact of Loneliness on Health Care Utilization Among Older Adults. Retrieved July 11, 2022, from https://ajph.aphapublications.org
12 https://www.sciencedirect.com/topics/medicine-and-dentistry/ucla-loneliness-scale